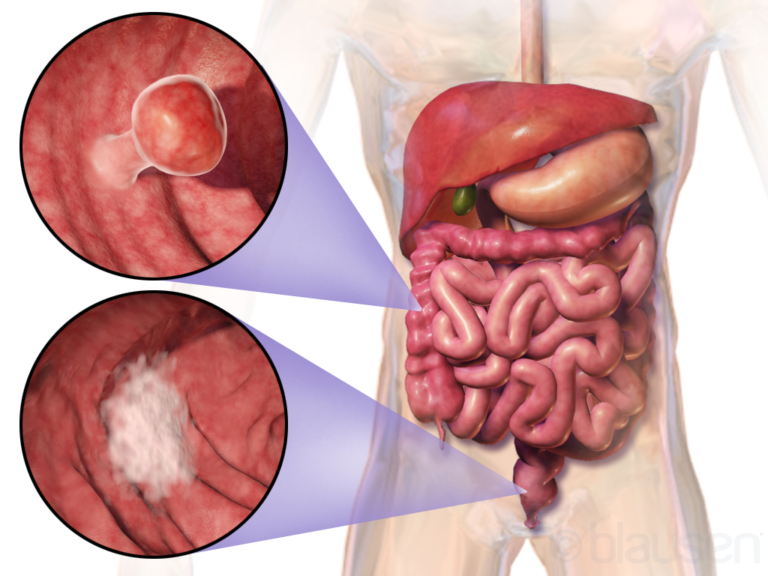
Treatment Options For Hepatobiliary Cancer
Hepatobiliary cancer, which encompasses cancers of the liver, bile ducts, and gallbladder, presents a formidable challenge in the field of oncology. Treatment strategies for hepatobiliary cancer have evolved significantly over the years, offering patients a range of options tailored to their specific condition and stage of disease. In this article, we delve into the various treatment modalities available for hepatobiliary cancer, highlighting advancements, challenges, and promising developments in the field.
To Know More About It Please Click Here
Surgery
Surgical intervention remains a cornerstone in the treatment of hepatobiliary cancer, particularly for early-stage tumors. Hepatectomy, or surgical removal of a portion of the liver, is often performed for hepatocellular carcinoma (HCC) and intrahepatic cholangiocarcinoma (ICC). In cases of localized bile duct cancer or gallbladder cancer, surgical resection of the affected organ may be pursued. Advances in surgical techniques, such as minimally invasive procedures and liver transplantation for select patients, have improved outcomes and expanded treatment options.
Chemotherapy
Chemotherapy plays a crucial role in the management of advanced hepatobiliary cancer, either as a primary treatment modality or in combination with other therapies. Traditional chemotherapy agents, such as gemcitabine, cisplatin, and fluoropyrimidines, have demonstrated efficacy in controlling tumor growth and improving survival outcomes. Additionally, targeted therapies, including tyrosine kinase inhibitors (e.g., sorafenib, lenvatinib) and immune checkpoint inhibitors (e.g., pembrolizumab, nivolumab), have emerged as promising options for patients with unresectable or recurrent disease.
Radiation Therapy
Radiation therapy, either alone or in combination with surgery and/or chemotherapy, is utilized in the management of hepatobiliary cancer to target tumors and reduce disease progression. External beam radiation therapy (EBRT) delivers high-energy X-ray beams to the tumor site, while techniques such as stereotactic body radiation therapy (SBRT) enable precise dose delivery to tumors with minimal damage to surrounding healthy tissue. Radioembolization, a form of internal radiation therapy, involves the delivery of radioactive microspheres directly into the blood vessels supplying the tumor, offering a localized treatment approach for unresectable liver tumors.
Interventional Radiology
Interventional radiology techniques play a vital role in the palliative management of hepatobiliary cancer, aiming to alleviate symptoms and improve the quality of life for patients with advanced disease. Procedures such as transarterial chemoembolization (TACE) and radiofrequency ablation (RFA) are utilized to target liver tumors and provide symptom relief by reducing tumor burden and vascular supply.
Clinical Trials and Emerging Therapies
The landscape of hepatobiliary cancer treatment is continually evolving, with ongoing research focused on identifying novel therapeutic targets and treatment strategies. Clinical trials evaluating innovative therapies, including targeted agents, immunotherapies, and combination regimens, offer hope for improved outcomes and personalized treatment approaches. Biomarker-driven trials seek to identify predictive markers of response to therapy, guiding treatment decisions and enhancing patient care.
Conclusion
The management of hepatobiliary cancer requires a multidisciplinary approach, incorporating surgery, systemic therapy, radiation therapy, and interventional techniques tailored to individual patient needs. Advances in treatment options, including targeted therapies and immunotherapies, hold promise for improving outcomes and quality of life for patients with hepatobiliary malignancies. Continued research and collaboration are essential in furthering our understanding of the disease and advancing the field of hepatobiliary oncology.